Featured
New Arrivals
OUR BLOGS
5
Sep
Sep
Antioxidant Food Supplements
Antioxidant supplements play a protective role for our general health including the h..
4
Apr
Apr
Belize Superfoods
We’ve all had days when we didn’t feel like we were ‘on our game.’ And as we age, bot..
27
Jan
Jan
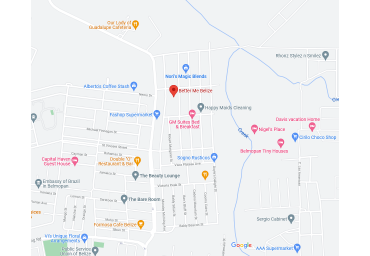
Better Me Belize New Location
Better Me Belize #35 Mount Mossey Street
..
7
Sep
Sep
Clearer Skin Belize
Well, I’m writing this because I know there are millions of people out
there with a..
18
Apr
Apr
High Intensity Interval Training and Intermittent ..
If you want to alter your body composition, you cannot overlook exercise.
However, ..